The following is a guest post by Dr. Vincent Guilamo-Ramos.
Dr. Guilamo-Ramos is the vice-chair of the Latino Commission on AIDS, and director and founder of the Center for Latino Adolescent and Family Health. He answered questions from Science Speaks on the impacts of the COVID-19 pandemic on Latinx populations in the United States.
Latinx communities have been described as bearing one of the heaviest burdens on the COVID-19 pandemic in this country. Can you quantify what that means?
It means that while Latinx people make up less than a fifth of the United States population, they account for nearly a third of people who have been confirmed to have COVID-19 here. Of the more than 100,000 people who have died from the coronavirus in the U.S., 26.9 percent were Latinx.
In New York State, which has received global attention as a COVID-19 hotspot and accounts for nearly a quarter of all people confirmed to have COVID-19 in the U.S., about 14% of people who have died from the disease are Latinx, even though Latinx people -- outside of New York City -- comprise about 12% of the state’s population. In New York City, home to more than half (53%) of all COVID-19 cases in New York State, Latinx people make up about 29 % of the population, and account for 30% of COVID-related deaths, which amounts to the highest rate of COVID-related deaths of all racial/ethnic groups in the city. Latinx also account for 30% of people confirmed to have COVID-19 who are not in the hospital, and 34% of non-fatal hospitalized COVID-19 patients in New York City.
Why is the pandemic having these harsh impacts – with higher incidence, severe illness and deaths among Latinx people?
Structural discrimination against Latinx and immigrant populations leads to lower pay, less employment security, access to healthcare and suboptimal housing options.
Let’s zero in on the Bronx, the New York City borough with the highest rate of COVID-19 diagnoses, and where more than half the residents identify as Latinx. The Bronx is the borough where I was born and have worked for more than two decades as a clinical researcher and more recently, as a nurse practitioner providing HIV prevention and treatment to adolescent and young adults. 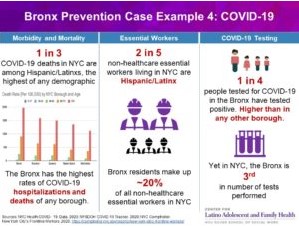
Bronx residents have the highest COVID-19 related hospitalization rates (634 per 100,000) in the city, and, one in five people to die of COVID-related causes in New York City are Bronx residents. Being Latinx and a Bronx resident raises risks of repeated exposures to the virus. More than half of New York City essential workers are foreign born and Bronx residents make up 17 percent of all frontline workers in New York City. Many of these essential and frontline workers continue to have limited access to personal protective equipment and options for physical distancing.
Then, when they get sick, their risks of severe illness and negative outcomes are higher.
The Bronx performs the worst compared to all four other NYC boroughs in elementary school absenteeism, educational attainment, rent burden, teen births, incarceration, and assault hospitalizations. With these social determinants of health, Bronx residents fare poorly on self-reported health, and life expectancy metrics. Many of the health issues that commonly accompany poverty are evident in the Bronx, which has among the highest rates of HIV infections in New York City, highest rate of asthma emergency visits in the state, the highest prevalence of diabetes, and the highest rates of obesity.
What can be done to reduce these impacts on Latinx populations?
Long and short term answers have to focus on tackling barriers to health care, and to improvements in Latinx social welfare . This means both local and federal policies ensuring that health services are immediately and reliably available to people in socioeconomically disadvantaged communities, including people who have emigrated to this country, who have unstable employment, and inflexible work conditions. The HIV pandemic, which also has had far disproportionate impacts in urban and rural economically disadvantaged communities such as the South Bronx where barriers to health services are high, has shown us the need for prevention and treatment services that meet the needs and circumstances of specific communities. Readily accessible testing, as well as inclusion in clinical trials for treatments and vaccines in hospitals serving economically disadvantaged areas, are critical now.
In this context, we also need to start thinking about innovative ways of delivering prevention and healthcare services in communities with access barriers to traditional service settings. We have seen a surge of remote health service delivery and telehealth, but there are limitations on the types of healthcare services that can be delivered remotely and stable internet access remains limited for some. An important next step is the development of novel healthcare service delivery systems that are directly based within and accessible to the communities they serve.
In addition, employers of people providing frontline services, including all positions in health care settings, as well as in retail, factory and food service, need to be held accountable for ensuring workers have access to appropriate personal protective equipment, have paid sick leave and are not penalized for using it – or offered any form of incentive to work when feeling unwell.
The COVID-19 pandemic has highlighted pre-existing inequities among Latinx populations that put their lives at needless risk and complicate effectively combating current, as well as future outbreaks. Lawmakers and public health leaders must address historical vulnerabilities in legislation targeting Latinx health coverage, immigrant rights and all forms of racism and discrimination.
Dr. Vincent Guilamo-Ramos is a professor at New York University and trained as a clinical social worker and nurse practitioner specializing in the health of adolescent and young adults. Dr. Guilamo-Ramos is certified by the American Academy of HIV Medicine as an HIV specialist and board certified HIV/AIDS nurse. In addition, Dr. Guilamo-Ramos is a member of PACHA and an HHS treatment guidelines member. He also serves as the vice-chair of the Latino Commission on AIDS, director and founder of the Center for Latino Adolescent and Family Health. He is a member of the HIV Medicine Association, which produces this blog, and a member of HIVMA's Ending the HIV Epidemic Working Group.
