The following is a guest post by Dr. Vincent Guilamo-Ramos.
Dr. Guilamo-Ramos is the vice-chair of the board of directors of the Latino Commission on AIDS, and director and founder of the Center for Latino Adolescent and Family Health. He answered questions from Science Speaks on the impacts of the COVID-19 pandemic on youth living with HIV in the United States.
From the first reports of the outbreak of a novel coronavirus in Wuhan, and of the first outbreak at a long-term care facility in Washington State, numbers indicated that older individuals were at the greatest risk of severe illness. Do we need to broaden our view of populations at greatest risks?
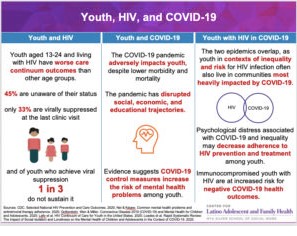
One concern is that key youth populations that may be at elevated risk have been largely overlooked. That includes youth with HIV, specifically those aged 13 to 24, who comprise 21 percent of all new HIV diagnoses in the United States, but because of their age, are not generally considered a population that is at significant risk of COVID-19.
The U.S. Centers for Disease Control and Prevention categorizes people with HIV who are not on antiretroviral treatment for HIV, and immunocompromised individuals, as a higher-risk group for negative COVID-19 related health outcomes.
The rates of HIV prevalence are highest among racial and ethnic marginalized populations and young men who have sex with men. Notably, youth have significantly worse outcomes across the HIV care continuum than their adult counterparts. Youth who are living with HIV are less likely to be diagnosed with HIV, and therefore less likely to receive effective treatment, with approximately 45% of youth living with HIV unaware of their HIV status.
Additionally, youth face greater challenges with HIV treatment adherence. While only 60% of youth diagnosed with HIV access treatment consistently and effectively enough to suppress the virus and protect their immune symptoms, less than any other age group, research has also shown that around one third of youth who achieve viral suppression do not sustain it. So, with disproportionately negative HIV care outcomes, youth with HIV may be at increased risk for negative COVID-19 related illness and death.
Do young people living with HIV face additional challenges in their daily lives as a result of the pandemic?
Many youths impacted by HIV already live in disadvantaged contexts that are amplified by COVID-19 control measures. Measures such as social distancing, shelter-in-place, and remote schooling have negatively disrupted the social, psychological, and educational trajectories of youth. Specifically, these COVID related public health measures can inadvertently increase adolescent risks of psychological distress, including depression and anxiety, domestic violence and youth maltreatment and add to obstacles to academic development challenges.
And while 35% of youth in the U.S. received their mental health services exclusively from school settings, school closures have disrupted this access.
You’ve indicated youth living with HIV already face obstacles to diagnosis, care and sustained treatment. How has the pandemic affected their already complicated service access issues?
In my experience as a nurse practitioner working with youth living with HIV and at-risk for HIV in the Bronx, there are noticeable effects the COVID-19 response has had on HIV care practices.
These include the accessibility of community-based organizations, medical offices, and primary care medical personnel. Many providers have switched to virtual care as an alternative, however, disadvantaged youths living with HIV may not have sufficient access to reliable internet or phone services to properly receive these services.
On the other hand, remote service delivery via telehealth has also resulted in the implementation of innovative service delivery models that remove historical barriers to youth accessing care. For example, pharmacy or mail delivery of prescription medications for 90 days, treatment of STIs through PO meds obtained at local pharmacies, patient triage without physical presence in clinical settings, etc. Some of these care delivery models may be applicable in the long-term, beyond the immediate COVID-19 response and warrant serious consideration as potential facilitators of the national plan to end the HIV/AIDS epidemic in the United States. Sorely needed is consideration of differentiated care models for HIV prevention and treatment of youth in the United States (see: https://nam.edu/shifting-the-paradigm-in-hiv-prevention-and-treatment-service-delivery-toward-differentiated-care-for-youth/).
Another point important to consider is that some youth living with HIV are also disproportionately affected by mental health and substance use disorders, which can be exacerbated by the psychological distress brought by COVID-19. And behavioral health issues, including depression, anxiety and alcohol and substance use have been linked to decreased adherence to HIV prevention and treatment.
It sounds like you are describing a pandemic within a pandemic.
I am. The Bronx, in New York is a borough with a large percentage of Latinx and black youth and significant HIV disparities. Currently, the Bronx is also the borough in New York with the highest rate of COVID-19 related deaths and illnesses. Efforts to maintain HIV prevention and treatment for youth with or at risk of HIV in the Bronx during the COVID-19 epidemic has been a priority for me.
Dr. Vincent Guilamo-Ramos is a professor at New York University and trained as a clinical social worker and nurse practitioner specializing in the health of adolescent and young adults. Dr. Guilamo-Ramos is certified by the American Academy of HIV Medicine as an HIV specialist and board-certified HIV/AIDS nurse. In addition, Dr. Guilamo-Ramos is a member of PACHA and an HHS treatment guidelines member. He also serves as the vice-chair of the board of directors of the Latino Commission on AIDS, director and founder of the Center for Latino Adolescent and Family Health. He is a member of the HIV Medicine Association, which produces this blog, and a member of HIVMA's Ending the HIV Epidemic Working Group.